Young kids aren’t immune: Mental health issues at crisis point amid lack of specialized therapists
| Published: 02-11-2024 12:10 PM |
Child therapist Alice Barber says that she could discharge all 45 of her clients — children as young as 2 or 3 years old — and her practice would fill back up within a couple of weeks, “no questions asked.”
Barber has colleagues who get 10 calls a week from parents hoping to get their young children enrolled in therapy but who can’t take any more clients because their schedules are already full.
“There’s this crisis that is happening that is absolutely overwhelming,” Barber said.
While the mental health crisis experienced by teenagers and adults has entered the spotlight in recent months, young children under the age of 12 are often left out of the discussion.
“The overarching belief is that young children are resilient,” said Barber, who runs a private practice in Easthampton and has worked in the field since the late 1990s. “In reality, older people are actually more resilient than younger children because younger children, their brains are still developing and are still so malleable that negative experiences can really have an impact on development.”
Before the COVID-19 pandemic, data from the Centers for Disease Control and Prevention found that nearly 20% of U.S. children ages 2 to 8 had a diagnosed mental, behavioral or developmental disorder. And since the pandemic, the number of children struggling with mental health problems has only grown, according to child therapists in the Pioneer Valley.
For children under the age of 12, mental health issues can look a little different than they might for teens and adults. While young children still struggle with anxiety, depression or stress, the way those conditions manifest is often behavioral — children experience sleep or eating disruptions, regress in potty training, become angry or irritable, struggle to follow rules or interact with peers and experience other symptoms.
“If we’re talking about the toddler age, they aren’t cognitively developed to the point that they have language for their emotions,” said Amanda Harrison, a Northampton-based counselor with more than two decades of experience in children’s mental health.
Article continues after...
Yesterday's Most Read Articles
 Local ‘Hands Off!’ standouts planned as part of national effort
Local ‘Hands Off!’ standouts planned as part of national effort
 Shelburne Selectboard determines police detective will retain job
Shelburne Selectboard determines police detective will retain job
 Local libraries react to state funding cuts, federal administrative leave
Local libraries react to state funding cuts, federal administrative leave
 Incandescent Brewing now open in Bernardston
Incandescent Brewing now open in Bernardston
 Cooking up an expansion: Cocina Lupita eyes second location in Turners Falls
Cooking up an expansion: Cocina Lupita eyes second location in Turners Falls
 ‘She is our future’: Thirty years after permitting women to join, Montague Elks is almost entirely women-led
‘She is our future’: Thirty years after permitting women to join, Montague Elks is almost entirely women-led
Harrison said that for some children, mental health problems are biological, while other times they are a response to traumas that the child has experienced, whether it is a direct trauma like abuse or neglect or the child is adjusting to a major life stressor such as divorce, separation, a move or a loss in the family.
“It’s our job to help them identify how they’re feeling, why they’re feeling that way and how they can shift that,” Harrison said.
To help kids work through their emotions, therapy sessions typically involve lots of creativity, play and toys.
“Children express themselves so much more eloquently and confidently through art and play and movement and dance and song,” Barber said. “They just don’t have the access to words that older people have.”
Barber sees children individually and also works with parents at the beginning and end of each session.
“There’s often a disconnect between how adults are responding to kids versus how they themselves would want to be responded to,” she said.
Carrie Joseph took her daughter to therapy with Barber at age 3 during her husband’s military deployment.
“She would go in alone and have her playtime with Alice; that’s all she really considered it,” Joseph said. “We did all this work to minimize any side effects … and she adjusted very well when he came home.
“I feel it is important for families to be in touch with their children and what their needs might be, especially in this time frame where life is so chaotic,” she added. “I think the kids are speaking to us, and I’m not sure the adults are always listening as well as they should.”
While the way children experience and deal with mental health struggles differs from older people, the causes behind the mental health crisis are largely the same across the board: increased screen time; identity and self-esteem issues, especially for LGBTQ and non-white children; substance abuse by parents and sometimes even children; academic stress at a younger and younger age; and concerns about large-scale issues like climate change and gun violence.
“All of these things, I don’t know how we could expect that the mental health of our very young children would be sound,” Barber said.
The COVID-19 pandemic has also taken a toll on the mental health of young children.
“We’ve never really seen anything like taking an entire generation of youth and entirely cutting them off from their social relationships, their ability to attend school [and] their ability to be part of a larger community,” Harrison said.
That social isolation, combined with the stress of having a serious illness in the community, family economic changes, and death and illness in the family, led to a “flood of kids coming into the emergency room” at Baystate Medical Center during the height of the pandemic, said Dr. Bruce Waslick, chief of child psychiatry at Baystate.
Over the last year or so, as kids have returned to school and the pandemic has receded, Waslick said Baystate is no longer seeing the same volume of kids boarding in the hospital for weeks before getting into programs.
“My sense is we’re getting back to the pre-pandemic levels,” Waslick said. “But the pre-pandemic state meant lots of kids with lots of mental health problems and probably not enough services to meet all the needs.
“Now it’s just a big problem instead of a really, really big problem,” Waslick added, downshifting to a “chronic crisis” level.
Workforce shortages are part of the problem. Barber said there aren’t enough therapists willing to work with young children because graduate schools don’t focus on very young children, and the work involves lots of playing, singing and “connecting with your own child self.”
At Baystate, Waslick said, “one strategy is we work closely with primary care doctors and pediatricians to help them feel confident to get involved with mental health problems with kids.” Primary care doctors are then able to recognize mental health issues, participate in treatment plans and collaborate closely with mental health professionals.
“What I see is a system that’s working really hard but just needs more support,” Harrison said. “We need a full community response. Ideally, we would have different levels of our community thinking, ‘What can we offer to help with this problem?’ ”
That community response would involve people donating their time or money to nonprofits or children’s mental health services; writing to state representatives and urging them to pass legislation to address the issue; and training more child therapists to join the workforce.
Parents have a role to play too, Harrison said.
“Increasing [parents’] abilities and their skills to really listen to their kids, validate how they’re feeling and then either meet their needs themselves or try and access someone to help,” she said. “I think a lot of parents have those innate skills, but I do think that we need more opportunities for parents to learn about children’s mental health.”
Talking about the problem and deflating the power of the word “resilient” when it comes to the mental health of children is a good first step, said Barber.
“I know it’s cliche, but it takes a village,” Barber said, “and if we are scared to access that village, then this is perpetuated that we are alone and stressed with our children who are struggling.
“Beginning to talk about this is what’s most important,” she added.








 New panel to review senior housing proposals in Deerfield
New panel to review senior housing proposals in Deerfield Shutesbury reviewing how to improve safety on Lake Wyola in wake of accident last summer
Shutesbury reviewing how to improve safety on Lake Wyola in wake of accident last summer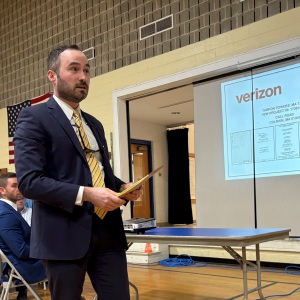 Colrain zoning board approves variance for Call Road cell tower
Colrain zoning board approves variance for Call Road cell tower
